That 1% Reduction Isn't Worth Your Salt: What a 30-Year-Old Study Still Teaches Us About Blood Pressure Interventions
When small numbers reveal big truths about where we should focus our health efforts
You'd think after decades of telling patients to cut their salt intake, we'd have rock-solid evidence that it makes a meaningful difference. But here's the thing—when you dig into the actual research, like this fascinating trial from the mid-90s called TONE (Trial of Nonpharmacologic Intervention in the Elderly), you start to wonder if we've been barking up the wrong tree.
"The trial tested whether weight loss or reduced sodium intake could maintain satisfactory blood pressure control after withdrawal of antihypertensive drug therapy in previously well-controlled, medicated hypertensives aged 60 to 80 years."
What's the Big Idea?
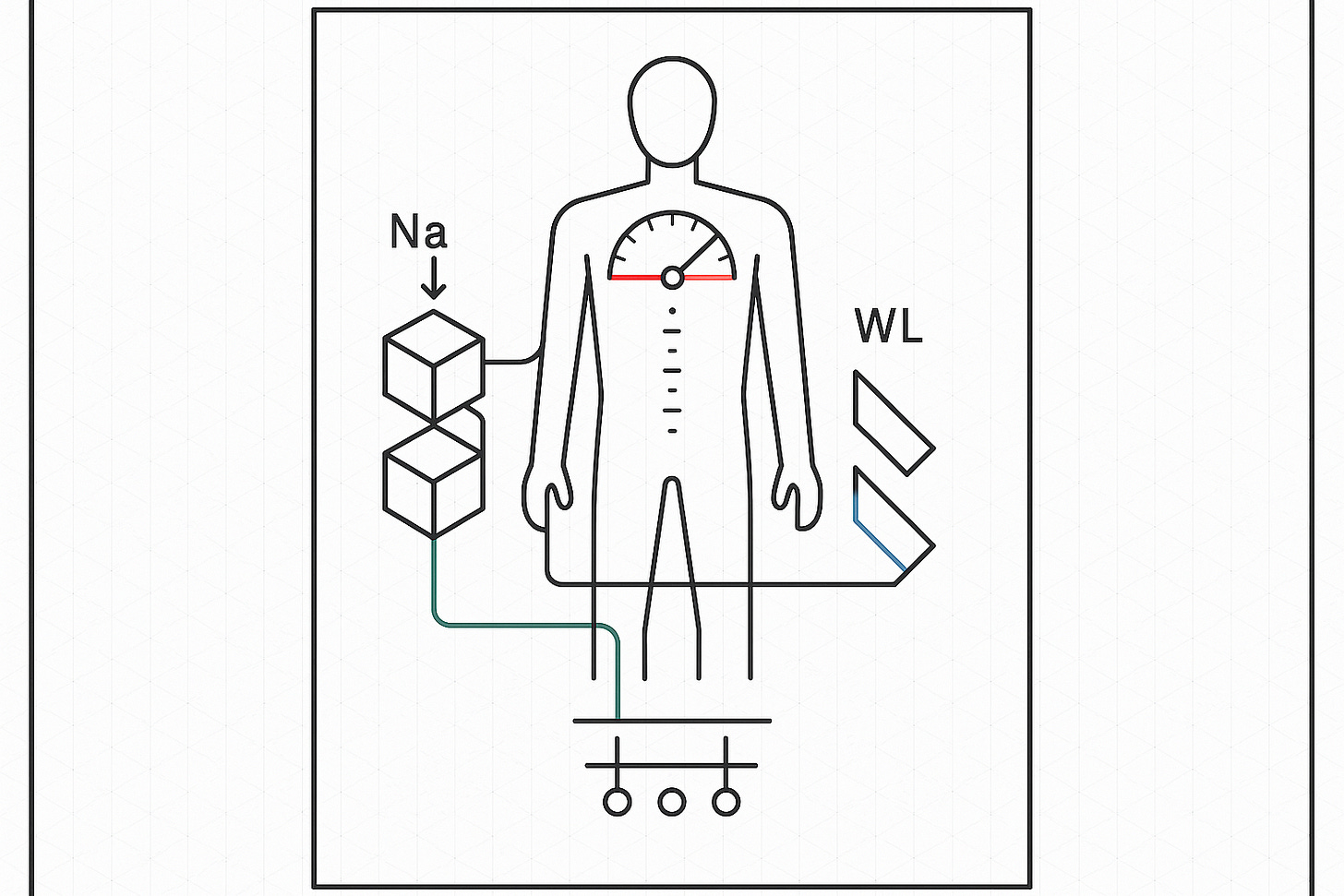
The TONE study tackled a question that still matters today: can lifestyle changes—specifically salt reduction and weight loss—help older adults manage their blood pressure without medication? Researchers recruited 900 people between 60 and 80 years old who were already on blood pressure meds. They split them into groups testing salt reduction, weight loss, both combined, or no changes at all.
Here's where it gets interesting. The study aimed for participants to cut their sodium to less than 80 mEq daily (that's about 1,800 mg) and achieve at least a 10-pound weight loss. After three months of lifestyle changes, they tried taking people off their blood pressure medications to see who could maintain healthy levels. Think about it—wouldn't it be great if we could ditch the pills?
But the targeted reductions tell a different story. They expected only a 25% reduction in the rate of returning to medication for the salt restriction group, compared to 30% for weight loss. And honestly, when you're talking about absolute benefits hovering around 1% in many cases, you've got to ask yourself: are we wasting precious time and energy on interventions that barely move the needle?
Why Should You Care?
Let's be real here. If you're spending months meticulously tracking every milligram of sodium, measuring your food, and turning down restaurant meals... for what amounts to a tiny reduction in blood pressure, maybe there's a better way. The study's own projections suggested that after 2.5 years, only about 25-30% of the control group would avoid returning to medication anyway.
The weight loss intervention showed slightly more promise than sodium reduction alone. But here's the kicker—the combined approach (both weight loss and salt reduction) was expected to show multiplicative benefits. In reality? The researchers even acknowledged potential "subadditive interaction," meaning combining interventions might not give you the bang for your buck you'd expect.
What really matters is this: while everyone's obsessing over their salt shaker, they might be missing interventions that pack a bigger punch. Exercise, for instance. A genuinely healthy diet pattern—not just low-sodium but rich in whole foods. These approaches don't just tweak one number; they transform entire metabolic profiles.
What's Next on the Horizon?
The TONE study wrapped up decades ago, but we're still having the same debates. Who knows, maybe soon we'll see more personalized approaches that identify which individuals actually respond meaningfully to sodium reduction versus those who don't. Some people are "salt-sensitive," others aren't—yet we give blanket advice to everyone.
The researchers were meticulous about their methodology, using 24-hour urine collections to verify sodium intake and elaborate behavioral modification programs. They met weekly, then biweekly, then monthly with participants. All that effort... and still, the expected benefits were modest at best. Makes you wonder if we could redirect those resources toward interventions with bigger payoffs.
Future research needs to get honest about effect sizes. Not just "statistically significant" reductions, but clinically meaningful ones. Because the difference between a systolic pressure of 148 versus 146? That's not changing anyone's life.
Safety, Ethics, and Caveats
Here's something the study did right—they carefully monitored participants as they came off medications, with weekly visits during the withdrawal period. They set clear safety thresholds (150/90 mm Hg) for resuming medication. No cowboy science here.
But there's an ethical dimension we need to consider. When we push marginally effective interventions on patients, we're not just wasting their time. We're potentially distracting them from changes that could genuinely transform their health. The study excluded people with serious conditions like recent strokes or heart attacks—exactly the folks who might need the most aggressive interventions.
The researchers also noted that maintaining these lifestyle changes required intensive support—introductory sessions, group meetings, individual counseling. That's a lot of healthcare resources for modest gains. Could those resources be better deployed? Almost certainly.
What This Could Mean for You
So where does this leave you if you're trying to manage your blood pressure? First, don't throw out everything you've heard about sodium—for some people, especially those with kidney issues or genuine salt sensitivity, it matters. But you might try prioritizing differently.
Instead of obsessing over every grain of salt, focus on interventions with proven, substantial benefits. Regular exercise—and I mean really regular, not just weekend warrior stuff—can drop blood pressure by clinically meaningful amounts. Weight loss, if you're overweight, tends to outperform sodium restriction. And here's a thought: stress management and sleep quality might matter more than that low-sodium label you're searching for at the grocery store.
Consider this: the TONE participants who managed to lose 10 pounds probably improved their blood pressure more through the weight loss itself than through any sodium changes. And they likely felt better overall, moved easier, and gained benefits that extended way beyond blood pressure.
The bottom line? Don't let perfect be the enemy of good. If cutting salt is easy for you, sure, go for it. But if you're struggling and stressed about sodium while ignoring exercise, sleep, and overall diet quality... well, you might want to reconsider your priorities. Sometimes the best medical advice isn't about doing everything—it's about doing the right things.