PNC-27: The Cancer-Killing Peptide That's Been Hiding in Plain Sight for Two Decades
Understanding how PNC-27 targets membrane proteins to trigger rapid cell collapse—and why it’s still flying under the radar.
Have you ever wished cancer treatments could function more like a sniper and less like a sledgehammer? This experimental peptide research is focused on exactly that—creating a “homing missile” mechanism that targets a specific weakness on the surface of tumor cells. The compound is called PNC-27. I actually first heard about this peptide on X and Reddit while I was frantically researching alternative options for a loved one.
It’s a strange feeling—seeing data that looks this promising and wondering why it hasn’t been front-page news for the last decade. The science detailed here describes a molecule that literally punches holes in cancer cell membranes while ignoring healthy tissue, a concept that sounds simple but requires complex molecular gymnastics.
“PNC-27... kills cancer, but not normal, cells by binding to HDM-2 associated with the plasma membrane and induces the formation of pores causing tumor cell lysis and necrosis.”
What’s the Big Idea?
The core innovation here is a peptide designed to exploit a misplaced protein found specifically on the surface of tumor cells. To understand how this works, you have to look at a protein called HDM-2. In healthy cells, HDM2 usually hangs out inside the cell or nucleus, regulating other proteins. But in many cancer cells, this protein strangely migrates to the outer surface—the cell membrane. It’s like a flag waving on the castle, signaling that something is wrong.
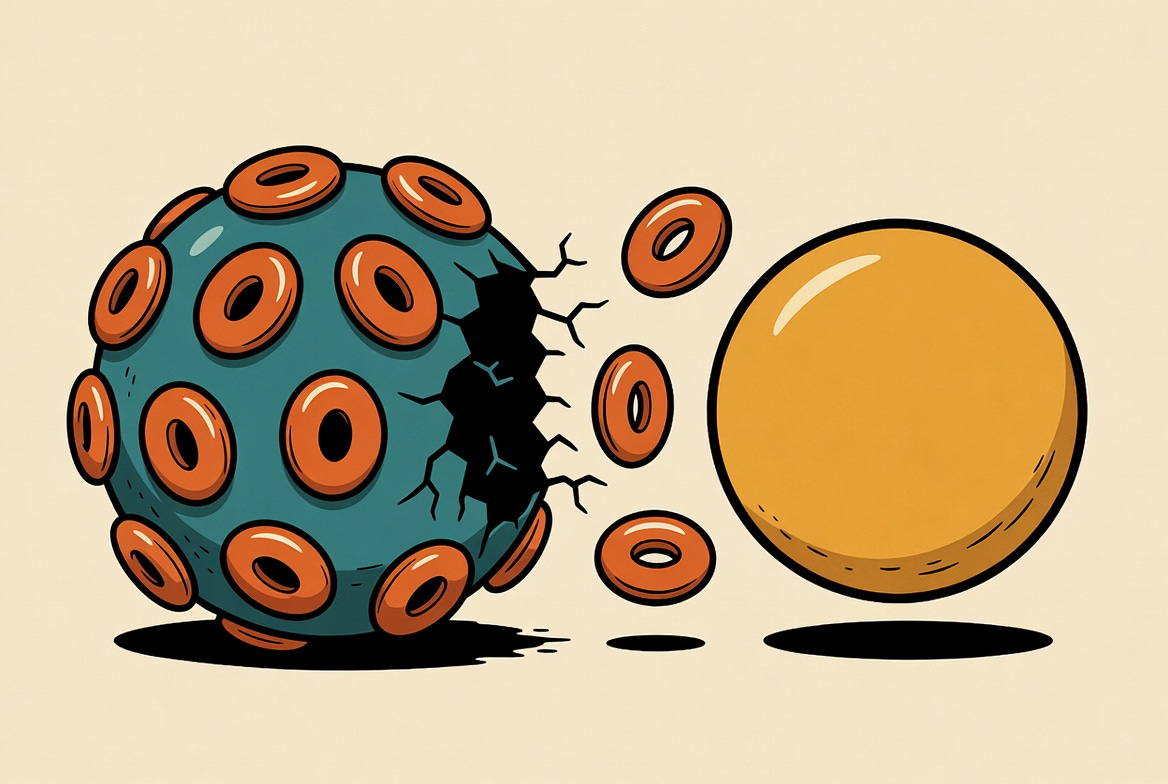
This paper analyzes how PNC-27, which is built from a piece of the p53 protein (often called the “guardian of the genome”) attached to a special delivery sequence, latches onto that exposed HDM-2. Once it binds, it doesn’t just sit there. It organizes into a ring shape.
Think about it like this: The peptide finds the target, calls its friends, and they link arms to form a literal donut shape on the cell surface. This “donut” is a transmembrane pore—a hole. Once that hole opens up, the cancer cell can’t control its internal environment anymore. It bursts and dies. This is known as necrosis. Honestly, given this clear mechanism, I’m disappointed but not entirely surprised that the peptide has received relatively little mainstream attention over the past few decades. It seems stuck in that valley between “promising lab result” and “pharmaceutical blockbuster.”
Why It Matters and What You Can Do
This approach to cell lysis is a departure from traditional treatments that often rely on triggering apoptosis, or programmed cell suicide. Cancer cells are notoriously tricky; they can often “turn off” their suicide switches to survive chemotherapy. PNC-27 bypasses that internal switchboard entirely. By physically breaching the hull of the cell, it causes destruction that the tumor can’t easily evolve to ignore.
Building on that, the selectivity reported here is what makes it so intriguing for longevity and healthspan enthusiasts. If you can remove senescent or cancerous cells without bathing the body in toxins, you preserve the overall system. However, since this is still in the research phase, the “what you can do” part requires a level head:
Monitor the mechanism, not the hype. Focus on therapies that target membrane-specific markers (HDM-2 in this case). This is likely where future breakthroughs will come from.
Understand the difference. Know that necrosis (messy cell death) and apoptosis (clean cell death) trigger different immune responses. This paper highlights necrosis, which can sometimes cause inflammation—a double-edged sword.
Avoid the “Grey Market” temptation. While there are vendors selling this online, and I definitely understand the desperation when looking for treatments for family, quality control is non-existent. If it’s indeed as effective as it seems, we need this standardized, not mixed in a bathtub.
What’s Next on the Horizon
The structural evidence is pointing toward a very specific physical interaction that requires body heat to work effectively. By using advanced imaging techniques like immuno-scanning electron microscopy, the researchers were able to actually see these pores. They found that the peptide and the cancer protein (HDM-2) link up in a 1:1 ratio to build these destructive rings.
From there, the data gets even more granular. The study showed that while the peptide binds to the cancer cell at cooler temperatures (like 17°C), the actual “drilling” of the hole depends on heat. It needs 37°C—body temperature—to let the molecules move around the membrane and assemble into those pores. This suggests that the therapy is tuned perfectly for human biology.
Moving forward, the obvious next step is moving from Petri dishes to proper human trials. The imaging proves the holes are real, and the chemistry explains why they form. Now, the challenge is delivery and stability in a living system. I would love to see this reach a wide range of people, but naturally, that can only happen after rigorous safety testing to ensure those “holes” don’t start appearing where we don’t want them.
Safety, Ethics, and Caveats
The safety profile discussed in this analysis is fundamentally linked to the presence—or absence—of that specific surface protein. PROOF of safety is just as important as proof of efficacy. The researchers tested PNC-27 on healthy human fibroblasts (connective tissue cells). Because these healthy cells keep their HDM-2 inside the cell rather than on the surface, the peptide had nothing to latch onto. No binding meant no pores, and the healthy cells remained completely intact.
However, we have to be realistic. This study was conducted in vitro (in glass/lab equipment). Living bodies are messy. Things that bind perfectly in a dish might get metabolized by the liver, or the immune system might attack the peptide before it reaches the tumor. Plus, inducing necrosis releases cellular debris, which can stress the kidneys or cause systemic shock if a large tumor dies too quickly. I see the massive appeal, especially compared to the “scorched earth” tactics of radiation, but balance is crucial. We need to verify that this specificity holds up when the complexity of a full human organism is introduced.
One Last Thing
It is fascinating to see physical evidence of a molecule that acts like a mechanical saboteur against cancer; keeping an eye on how these membrane-targeting peptides evolve could offer a glimpse into the future of precision medicine.
Explore the Full Study
Sarafraz-Yazdi, E., et al. PNC-27, a Chimeric p53-Penetratin Peptide Binds to HDM-2 in a p53 Peptide-like Structure, Induces Selective Membrane-Pore Formation and Leads to Cancer Cell Lysis. Biomedicines 2022, 10, 945. DOI: 10.3390/biomedicines10050945