When Cancer Treatment Breaks Hearts: The Hidden Cardiovascular Crisis in Breast Cancer Care
A comprehensive new review reveals why protecting the heart during breast cancer treatment is becoming as crucial as fighting the cancer itself.
Here's a sobering reality: while we've gotten remarkably good at beating breast cancer—with mortality rates dropping by 42% since 1989—we're discovering that the treatments saving lives are sometimes breaking hearts, quite literally. A groundbreaking review published in ESMO Open reveals that cardiovascular disease has now overtaken cancer as the leading cause of death in long-term breast cancer survivors, fundamentally shifting how we need to think about cancer care.
"A drug is only useful if people can tolerate taking it—and with discontinuation rates for hormone-blocking therapies reaching as high as 50% in some studies, current breast cancer treatments clearly aren't meeting that bar for many patients."
What's the Big Idea?
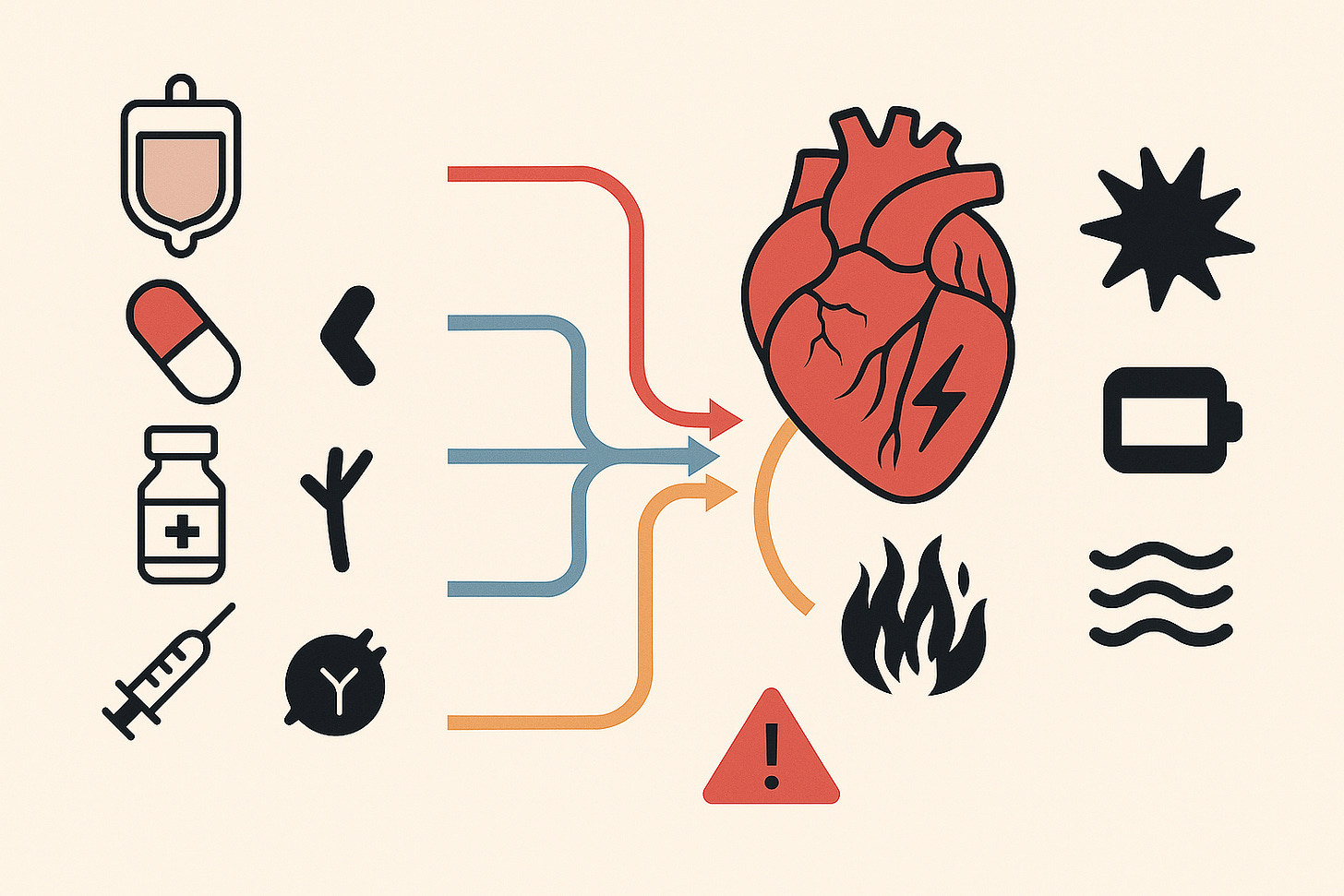
The research team, led by C. Dauccia and colleagues from major cancer centers across Europe and North America, conducted an extensive analysis of cardiovascular toxicity across the entire spectrum of modern breast cancer treatments. Their findings paint a complex picture: virtually every major class of breast cancer therapy—from traditional chemotherapy to cutting-edge immunotherapies—carries some risk of heart damage.
The mechanisms are as varied as the treatments themselves. Anthracyclines, the workhorses of chemotherapy, generate toxic oxygen species that damage heart muscle cells. Trastuzumab and other HER2-targeted therapies disrupt critical cardiac signaling pathways. Even hormone therapies, which many consider relatively benign, can increase risks of blood clots and heart problems through estrogen depletion.
What makes this particularly challenging is something I've observed in practice: the cardiovascular effects aren't always immediate or obvious. While some patients develop heart problems during treatment, others may not manifest symptoms until years or even decades later. The research shows that these delayed effects are especially common with anthracyclines and radiation therapy, creating a ticking time bomb that requires long-term vigilance.
Why Should You Care?
The implications extend far beyond the oncology ward. For the millions of breast cancer survivors worldwide, this research fundamentally changes the conversation about long-term health management. The study reveals that breast cancer survivors who received cardiotoxic treatments face increased heart failure risk regardless of their baseline heart function—meaning even those with perfectly normal hearts before treatment need ongoing monitoring.
Here's where it gets particularly frustrating from a clinical perspective: we're seeing that both chemotherapy and endocrine therapy often cause enough cardiotoxicity that the overall survival benefits become less clear-cut. As predictive models like Breast Predict improve, these survival advantages continue to shrink. And that's not even accounting for the quality-of-life issues with endocrine therapy—memory problems, mood changes, hot flashes, vaginal atrophy, and more. It turns out estrogen is quite important for overall health, and we desperately need better therapies that women can actually tolerate taking.
The statistics are stark: discontinuation rates for hormone-blocking drugs like SERMs and aromatase inhibitors reach as high as 50% in some studies. A drug is only useful if people can tolerate taking it, and current options clearly aren't meeting that bar for many patients.
What's Next on the Horizon?
The research points to several promising developments. The field of cardio-oncology—barely a decade old as a formal specialty—is rapidly evolving with new protective strategies. SGLT2 inhibitors, originally developed for diabetes, show remarkable promise in protecting hearts during cancer treatment. Multiple clinical trials are testing whether drugs like empagliflozin can prevent chemotherapy-induced heart damage.
Advanced imaging techniques are revolutionizing early detection. Global longitudinal strain (GLS) measurements can now detect subtle heart changes before traditional metrics like ejection fraction show problems. New cardiac MRI technologies can complete detailed assessments in just 10-15 minutes, making comprehensive monitoring more practical.
The study also highlights the potential of personalized risk assessment tools. The Heart Failure Association-International Cardio-Oncology Society (HFA-ICOS) scoring system helps identify high-risk patients before treatment begins, though real-world validation is still ongoing. As one researcher noted, this represents a shift from reactive to proactive cardiac care in oncology.
Looking ahead, I believe we'll need to completely rethink how we develop cancer therapies. The current model of prioritizing efficacy over tolerability simply isn't sustainable when half of patients stop taking their medications due to side effects.
Safety, Ethics, and Caveats
The review doesn't sugarcoat the challenges. Many cardioprotective strategies that showed promise in early studies have failed in larger trials. Statins, for instance, produced mixed results across different studies. Beta-blockers and ACE inhibitors showed only modest benefits in preventing heart damage.
There's also the ethical dilemma of treatment decisions. How do you balance aggressive cancer treatment against long-term heart risks? The authors emphasize that this requires honest conversations between oncologists, cardiologists, and patients about individual risk factors and life goals. One concerning finding: most clinical trials of newer cancer drugs exclude patients with cardiovascular risk factors, meaning real-world toxicity rates are likely higher than reported.
Perhaps most troubling is what we don't know. The review reveals significant gaps in understanding late cardiovascular effects, particularly for newer targeted therapies and immunotherapies. We're essentially conducting a massive uncontrolled experiment on millions of cancer survivors. While the immediate priority remains treating the cancer, we can't ignore that we're potentially trading one life-threatening condition for another.
What This Could Mean for You
If you're facing breast cancer treatment or are a survivor, this research underscores several critical action points. First, comprehensive cardiovascular assessment before starting treatment isn't optional—it's essential. This includes not just an EKG but potentially echocardiography and biomarker testing.
During treatment, don't dismiss symptoms like shortness of breath, fatigue, or swelling as "just side effects." These could signal developing heart problems that need immediate attention. The research shows early detection and treatment of cardiotoxicity dramatically improves outcomes.
For survivors, long-term cardiac monitoring should be part of your care plan. The study recommends periodic heart function assessments during the first year after treatment completion, with ongoing annual evaluations for high-risk patients. Lifestyle modifications—regular exercise, heart-healthy diet, blood pressure control—become even more critical.
Given the high discontinuation rates of current therapies, particularly hormone treatments, work closely with your oncology team to find tolerable options. Don't suffer in silence—if side effects are unbearable, speak up. Your medical team can only help if they know you're struggling, and there may be alternatives or supportive care options available.
Most importantly, advocate for coordinated care between your oncologist and a cardiologist familiar with cancer treatment effects. The emerging field of cardio-oncology exists specifically to bridge this gap, though access remains limited in many areas.